Turning a Denial Pattern into Predictive Power
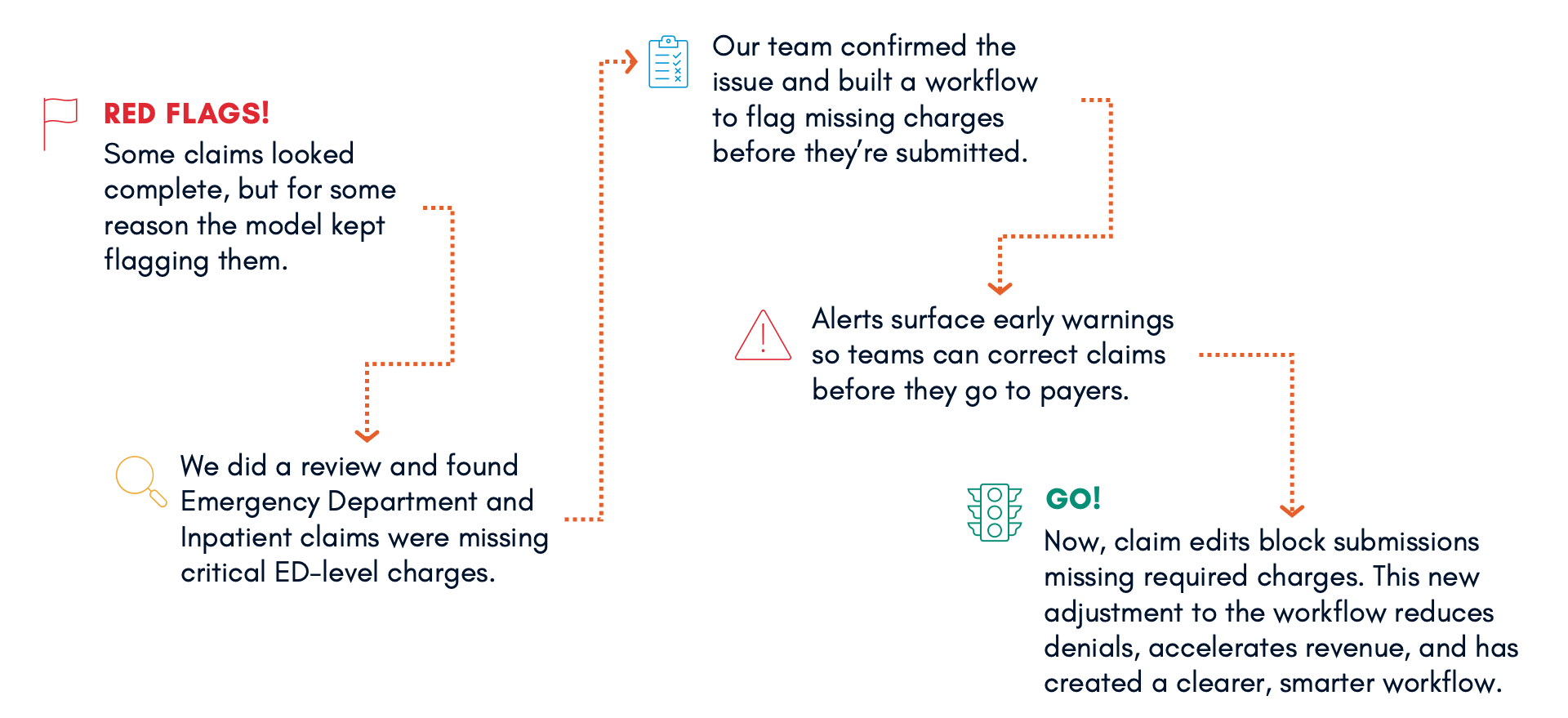
It all began with a few claims that didn't seem quite right. One of our predictive denial models was flagging accounts that, on the surface, appeared complete. The data looked clean, and the claims seemed ready for submission. However, the model consistently identified them, indicating that something was off.
As our team investigated, the pattern became apparent. These were Emergency Department (ED) and Inpatient claims that were missing a critical detail: the ED charge. Without this essential information, those claims were destined for denial. This issue was not isolated; across several clients, we started noticing the same trend. In one organization alone, we identified approximately $1.7 million in missing revenue for the ED-level charges.
We took these insights and took immediate action. We developed a workflow in our Revenue Integrity dashboard to flag these cases early, well before claims are generated. This workflow now ensures the issue is visible and actionable, allowing teams to correct it before the claim is submitted to the payer.
The next step is to implement a claim edit that prevents any claim from being submitted without the appropriate revenue code charge. This action effectively connects predictive intelligence with process design. Our ultimate goal is to catch what's missing before it becomes a problem and keep avoidable denials out of the revenue cycle.
This progress exemplifies what effective AI should look like in healthcare. It doesn't replace people or make decisions in isolation; instead, it highlights important issues, connects insights to action, and enables teams to work more efficiently. It transforms data into foresight and insights into protection.
When AI is designed to support the workflow, rather than the other way around, it creates clarity, accuracy, and better outcomes across the entire revenue cycle. This is the advancement we have been striving for and the change we're trying to spark.
AI Is the Foundation, Not an Add-On
Most “AI” in healthcare is flashy marketing with little impact. At SparkChange, AI is the foundation of everything we do. It powers actionable, transparent intelligence that enables revenue cycle teams to work smarter, make faster decisions, and prevent issues before they occur.
Our approach combines analytics, automation, and services. Analytics provide visibility into every step of the revenue cycle, surfacing trends, anomalies, and opportunities that teams can act on immediately. Automation removes repetitive, error-prone work and accelerates critical processes, freeing staff to focus on higher-value tasks. Services ensure that insights and automations are implemented effectively, workflows are optimized, and improvements are sustainable over time.
By building AI into the foundation — not layering it on top — we create systems that deliver measurable impact every day, improve accuracy, reduce delays, and strengthen the overall revenue cycle. This is how intelligence becomes operational, how insight drives action, and how AI truly works for people.